In a smoothly functioning billing and claims world where all the stars, motives, and players align, a patient and a surgeon would agree upon a medically necessary course of treatment and the third party payer or contract (assuming there is one) would be consulted for reimbursement amounts. The patient and surgeon then schedule the procedure, complete it, submit the claim and are paid the agreed upon amount within a few business days. In a perfect world, from the provider’s perspective, they could even be paid a portion upfront to cover pre-op costs.
The technology is here to do all of that…and more. This is not a technology problem. It’s an alignment problem that has turned into an inordinately complex process filled with legal potholes.
You may have seen AT&T’s Just OK commercials. Whatever your experience with AT&T, these commercials make a great point about tried and true expertise – about putting in the time to be excellent – “Just OK is not OK.” All of the surgeons we work with have dedicated the time and effort required in their craft in order to serve their patients well. No one imagines placing their lives in the hands of a surgeon who hasn’t. Shouldn’t surgeons want the same thing they offer their patients when it comes to tried and true expertise in handling their claims and appeals so they have great reimbursement outcomes to match their patients’ great surgical outcomes?
As a business that serves the surgical needs of patients, a surgery center must focus from the ground up on how they are going to provide the absolute best surgical experience for their patients in the communities in which they serve. Reimbursements are important, but they are of secondary importance to the main work of the surgery center…to perform excellent surgeries so patients get back to living.
The alignment problem between providers and payers isn’t going away as long as we have a third-party payer system. The order of complexity keeps growing annually as it has for decades. The complexity now entails coding, bill formatting, state statutes, federal laws (HIPAA, ERISA, PPACA), specific insurer procedures, employer connections, data and predictive modeling, in-network and out-of-network differences, as well as patient education, engagement, and advocacy. Like a surgery center, command mastery of this kind of process detail means building a business for this, and only this, from the ground up.
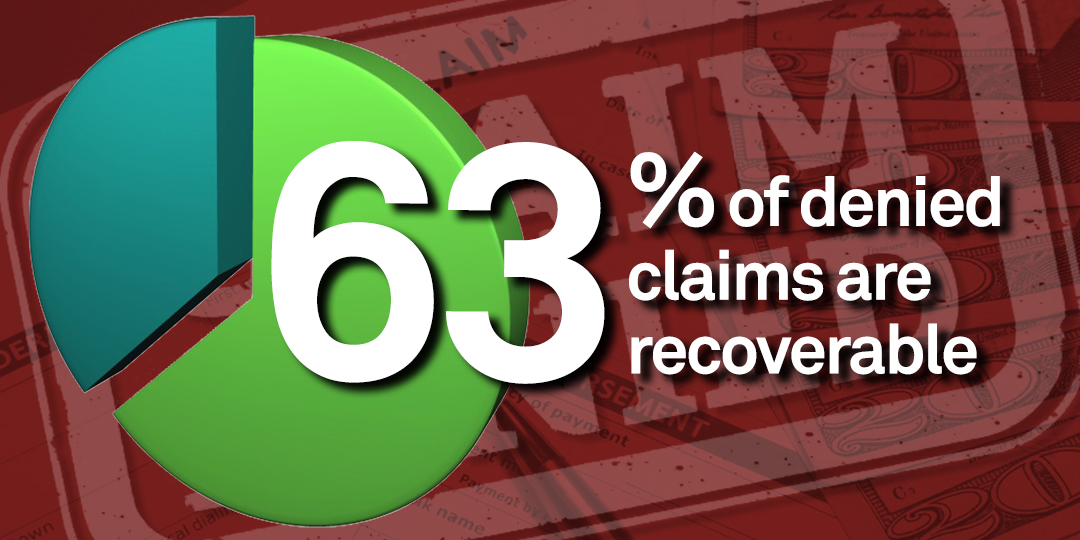
Research in 2017 demonstrates that they typical health system risks nearly $5 million each year due to claims denials alone. Nine percent of hospital charges are denied initially. Your claims denials experience at your surgery center may be even higher. What do you do with denied claims? Do you have a functioning, effective appeals process? Hospitals are seeing that up to 63% of denied claims are recoverable. Isn’t that 63% potential alone worth doing a strategy check with an expert?