GROWING REVENUE FOR OUT-OF-NETWORK PROVIDERS
- Expert application of the claims and appeals process boosts reimbursements.
- Predictive modeling provides pinpointed payment projections to maximize profitability.
- Highly effective deductible and co-insurance management increases cash flow, mitigates provider risk, and preserves patient commitment to move forward with treatment.
- Intelligent utilization of legal resources ensures optimal reimbursements.
PROVIDING BOTH PATIENT-CENTRIC AND DATA-BASED SOLUTIONS
- A team of professional patient advocates ensures that patients understand their plan, are informed of the process, and feel good about utilizing the benefits they invested in.
- Forensic financial analysis on each plan allows providers to make data-driven decisions to maximize profitability of surgical cases.
- Data analysis and proprietary algorithms enable highly accurate financial forecasting, so providers know in advance the amounts they are likely to be reimbursed, removing the guesswork from out-of-network reimbursements.
MITIGATING RISK THROUGH KNOWLEDGE AND COMPLIANCE
- Command mastery of federal and state law coupled with a highly analytical predictive approach allows providers to focus on delivery of care while Contego focuses on financial returns.
- Attorney engagement with plan fiduciaries ensures that benefits are paid according to plan.
- Continual engagement with top healthcare attorneys ensures processes are constantly adapting to market realities as well as compliant with state and federal law.
Contego optimizes financial outcomes for providers by advocating for patients so they receive the care they’ve been paying for.
HOW CONTEGO GETS PROVIDERS PAID
- By unlocking the value of the ASC as a revenue generator.
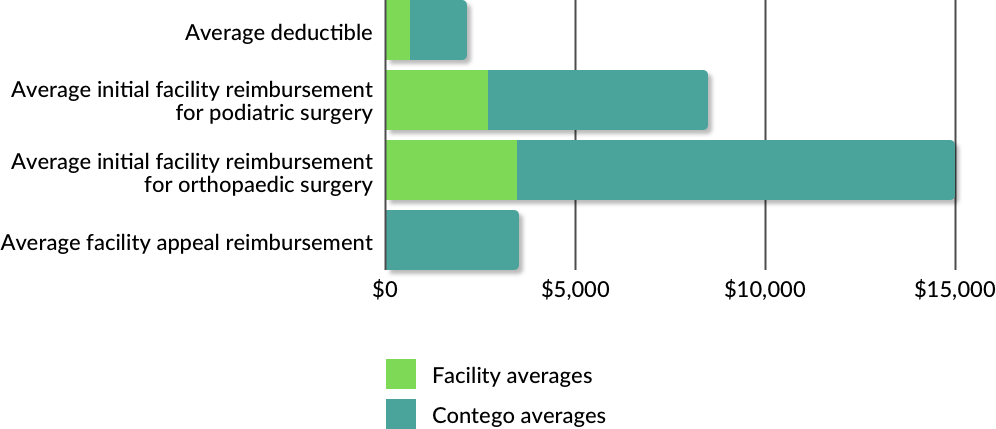
- By maximizing multiple revenue channels per medical event. (Deductible, Claim, Appeal, Co-Insurance)
- By optimizing capacity utilization through pre-surgical plan and benefits analysis.
- By engaging employer plan administrators as fiduciaries in the process.
- By leveraging data to negotiate settlements with carriers.