ASC Industry Awareness
ASCs Save Hassle, Time, and Money
ASCs/OBSs/OBLs and all their surgery center cousins have a tremendous impact upon total patient well-being. Convenience, ease of use, surgery safety, and lower cost are all benefits achieved due to selecting an ASC for surgical procedures where feasible. Shifting common outpatient procedures to ASCs also yields savings for the US healthcare system. Even Medicare saves $4.2 billion annually due to ASCs. ASCs with twenty-five or more orthopaedic cases per month are positioned best to thrive so that everyone in the surgery center ecosystem wins.
ASC Physician Ownership Strength
Even with all the chatter around consolidation, 52% of ASCs are still 100% physician-owned. Physician ownership enables surgeons to schedule procedures more effectively and efficiently, grants maximum control over the operating room environment, and creates more responsiveness to specific patients’ needs. Declining physician pay in both inpatient and outpatient settings makes the benefits of working in ASCs that much clearer. Medscape’s 2022 Compensation Overview demonstrates that self-employed physicians earn 20% more than employed physicians do. These are among the factors that make ASCs resistant to widespread consolidation.
Healthcare Industry/Trends
Prior Authorization Reform
Prior authorization reform momentum is growing. Pennsylvania is the latest of three states taking on reform measures in 2022. November 3, Pennsylvania Governor Tom Wolf signed Act 146 of 2022 into law, which seeks to drive better patient outcomes by expediting treatment plans in all commercial and Medicaid plans. The law will enable the creation of a standardized electronic portal to push through barriers that typically devolve into treatment delays (infographic), streamlining the process and making it more transparent. Earlier this fall, the US House passed a bill to install electronic prior authorization in Medicare Advantage plans. The AMA has been convening provider stakeholders and keeping pressure on prior authorization reform. Pennsylvania’s success will help to fuel efforts at the state and federal levels.
2022 and 2023 Financially Challenging for Many Hospitals
Inflation continues to squeeze hospital margins, which have been running negative for the bulk of 2022. More aggressive patient cost sharing through high-deductible health plans, labor shortages, and contracted rates that undershoot costs are all playing havoc with smaller, typically rural, hospitals. Over 600 rural hospitals are at risk of closure, 200 of them are at immediate risk with very low financial reserves. Chapter 11 healthcare bankruptcy filings are 28% higher in 2022 than in 2021, though that number is inflated since 2021 bankruptcies were off by 44% from the previous year. As pandemic safety nets drop and funding sources grant fewer financial extensions, hospital closures and bankruptcies are expected to continue to spike in 2023.
Healthcare Digital Transformation Watch
What Will the Eventual End of PHE Mean for Telehealth?
This is a question without a definitive answer at this stage. On October 13, 2022, Xavier Becerra, US Secretary of Health and Human Services, renewed the January 31, 2020-initiated COVID-19 public health emergency (PHE), which will remain in effect until January 11, 2023. The PHEs have enabled extended use of telehealth services. At some point, the COVID-19 PHEs will no longer be renewed – raising questions about future telehealth access and coverage. States vary in their approaches to telehealth coverage requirements for both public and private health plans, including eligibility for reimbursement. As an amendment to ERISA, H.R. 7353 – Telehealth Benefit Expansion for Workers Act of 2022 was introduced at the end of March to treat telehealth services in group health insurance coverage as accepted benefits.
Healthcare M&A, Valuation, Revenue Cycle
Provider Challenges with RCM
Increasing denials and unfavorable payer mixes are among healthcare providers’ top revenue cycle management concerns. Staffing challenges are also significant. So much so, that RCM is now the most common area for hospital leaders to outsource. Whether providers keep the RCM function in house or they work with an RCM partner, like Contego Solutions, is a big decision that can significantly affect reimbursements and revenue. Increasingly, automation in medical billing is also enabling RCM as a service options.
Out-of-Network Watch
NSA’s IDR Challenges Continue
On August 19, HHS and The Department of Labor (DOL) released the NSA Final Rule, which was set to take effect on October 25, 2022. In September, the Texas Medical Association (which, in 2021, issued the first successful challenge to the Independent Dispute Resolution process) issued a new lawsuit, challenging the amount of emphasis placed on the qualifying amount, because it would ultimately create a financial incentive imbalance between providers and insurers. ER, radiology, and anesthesiology societies are supporting the suit, as are the AHA and AMA. Interestingly, some state resolutions have not adopted the federal final rule and have processes that are more favorable to providers.
Legal
What Is New for Open Enrollment Season This Year?
From the office of Jon Sistare, JD, Attorney at Law
It is open enrollment season for health insurance at companies throughout the US, and employers are providing more options with low or no deductibles to try to make plans more affordable for employees.
That is one of the top findings of surveys conducted by benefit consultants for the 2023 plan year. More than 40% of large employers surveyed by Mercer said they will provide a plan with a low or no deductible in 2023, such as a copay-based plan, and 11% are considering it, the professional services firm reported. About one in five large employers said they are focusing on enhancing benefits for their hourly and low-wage workers.
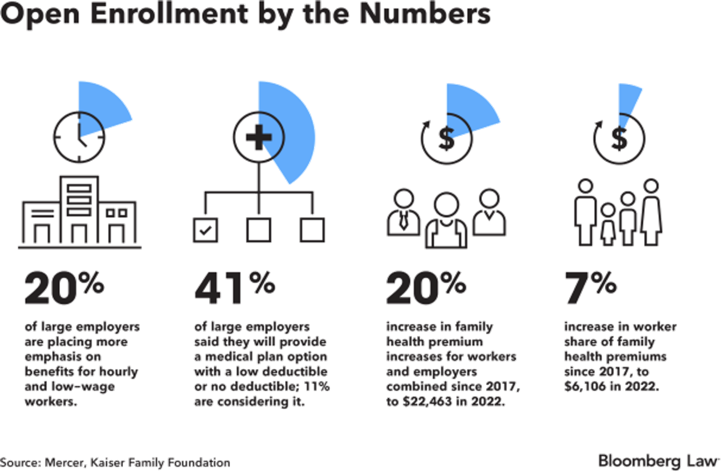
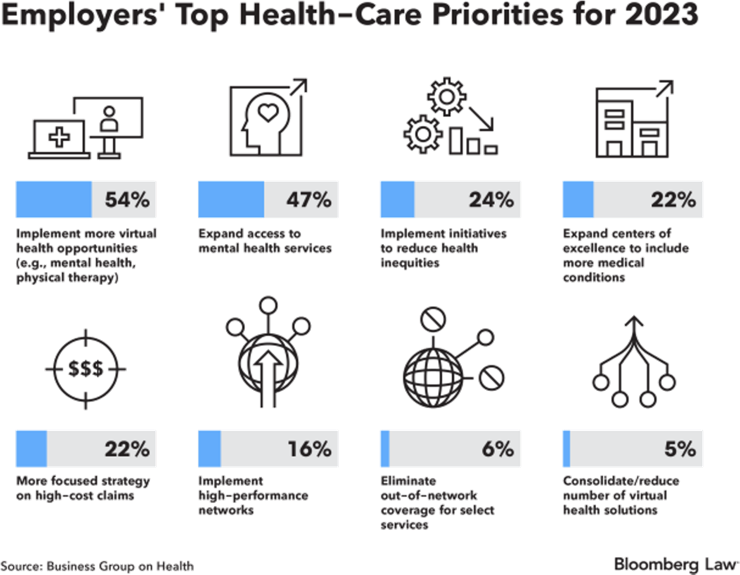
Annual family premiums stayed nearly flat in 2022 at $22,463, but the Kaiser Family Foundation said recent inflation suggests that larger increases are “imminent.” Employers are also trying to rein in costs by implementing more virtual health opportunities and expanding the use of centers of excellence for more conditions, such as cancer. Additionally, expanding access to mental health services is a high priority for many, with 47% of employers listing that as a top priority.
At a Glance
What to Know about CMS’ Final Payment Rules for 2023
Physician Fee Cut and Home Health Boost
New Study on Brain Lucidity Advances Understanding
Does Brain Function Cease at Cardiac Death?
Newsweek: America’s Best ASCs 2023
State-by-State Rankings
HCA Revenue and Profit Slipped in Q3
Many in Healthcare Found a Fiscally Challenging Q3
Banner/Aetna Introduce “Frictionless Billing”
Partnership Seeks to Ease Claims Process for Banner Health Members
To subscribe or unsubscribe to ASCs in Motion, simply send an email request to levans@contegollc.com.
To inquire about Contego’s expert reimbursement solutions:
Call 855.505.8346 x1245 or Email info@contegollc.com
Contego Solutions, LLC
https://contegollc.com
https://www.linkedin.com/company/contego-solutions-llc/
